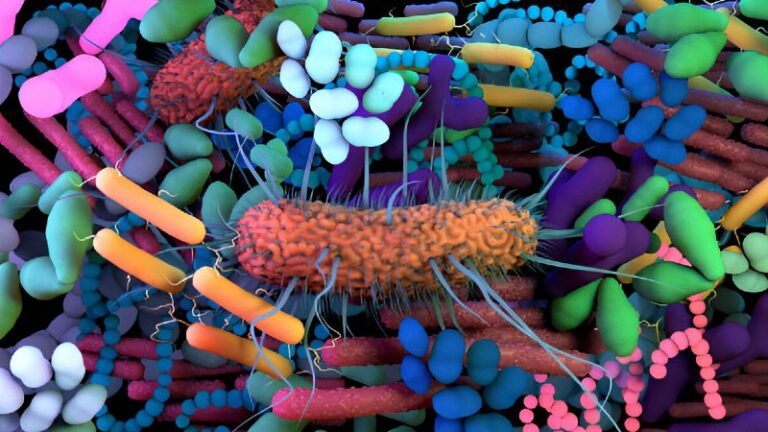
The human body is home to trillions of microbes bacteria, viruses, fungi, and archaea that collectively form the human microbiome. Far from being passive passengers, these microorganisms act like an internal ecosystem, influencing everything from digestion to immunity and even mental health. In recent years, microbiome science has shifted from cataloging microbial species to exploring how these microbes function, adapt, and co-evolve with us throughout life. This perspective is transforming medicine, nutrition, and preventive healthcare.
What Is the Human Microbiome?
The term microbiome refers to the entire community of microbes living in and on the human body. These microbes are found in:
- Gut: The largest and most diverse microbial hub.
- Skin: Protects against pathogens and helps regulate the immune system.
- Oral cavity: Involved in digestion and oral health.
- Respiratory tract: Influences immune responses to infections.
- Urogenital tract: Maintains reproductive and urinary health.
Collectively, the microbiome contains over 150 times more genetic material than the human genome, making it a second genome that dramatically expands our biological potential.
Why Microbiomes Matter
While the gut microbiome is best known for aiding digestion, its influence extends much further:
1. Immune System Training
Microbes educate immune cells, teaching them to distinguish between friend and foe. For example, certain gut bacteria promote regulatory T cells that prevent autoimmune overreactions.
2. Metabolic Regulation
Microbial metabolites such as short-chain fatty acids (SCFAs) like butyrate reduce inflammation, strengthen the gut barrier, and improve insulin sensitivity.
3. Neurological Connections
The gut-brain axis shows how microbiota influence mood and cognition. Studies link gut dysbiosis with anxiety, depression, and even neurodegenerative diseases like Parkinson’s.
4. Protection Against Pathogens
Healthy microbes act as gatekeepers, occupying niches that harmful bacteria might exploit. For instance, vaginal microbiota dominated by Lactobacillus crispatus reduce risk of preterm birth.
Microbiomes Across the Human Lifespan
One fresh way to understand microbiomes is to see them as co-evolving ecosystems that shift with us at each stage of life:
| Life Stage | Microbiome Characteristics | Health Implications |
|---|---|---|
| Infancy | Seeded during birth (vaginal or C-section), shaped by breastfeeding. | Early composition affects allergies, asthma, and immunity. |
| Childhood | Diversifies with diet and environmental exposure. | Key for immune system training and resilience. |
| Adulthood | Stable but shaped by diet, stress, and lifestyle. | Imbalances linked to obesity, diabetes, and gut disorders. |
| Older Age | Reduced diversity and beneficial bacteria. | Associated with frailty, inflammation, and neurodegeneration. |
Examples of Microbiome-Health Connections
Preterm Birth
Research shows African-American women with reduced Lactobacillus crispatus in early pregnancy had higher risk of preterm birth. Detecting these shifts may allow for early interventions.
Inflammatory Bowel Disease (IBD)
Patients with Crohn’s disease or ulcerative colitis often lose anti-inflammatory bacteria like F. prausnitzii and R. hominis. This reduces butyrate levels, weakening gut defenses and worsening inflammation.
Type 2 Diabetes (T2D)
Prediabetic individuals show distinctive microbiome profiles that affect immunity and metabolism. Intriguingly, flu vaccination improved immune responses in these patients, suggesting that microbiome-linked immunity influences disease progression.
Factors Shaping the Microbiome
Several lifestyle and genetic factors determine microbiome composition:
- Diet: Fiber-rich diets increase diversity; high-fat, low-fiber diets promote dysbiosis.
- Antibiotics: Early and repeated use disrupts microbiome balance.
- Stress & Sleep: Stress hormones and poor sleep alter gut microbial stability.
- Environment: Urban living vs. rural exposure creates distinct microbiome patterns.
- Genetics: Host genes like FUT2 and NOD2 influence microbiome susceptibility to disease.
Microbiomes as Personalized Medicine Tools
With advances in multi-omics (genomics, metabolomics, proteomics), researchers can now track not just which microbes are present, but what they do. This is driving new opportunities:
- Predictive biomarkers: Early microbiome shifts could warn of diseases like diabetes or IBD.
- Targeted therapies: Probiotics, prebiotics, or even fecal microbiota transplants (FMT) to restore balance.
- Precision nutrition: Tailoring diets based on microbiome composition to optimize health.
- Immune support: Using microbiome signatures to predict vaccine effectiveness.
Microbiomes as Dynamic Ecosystems
A fresh way to view the microbiome is not as a fixed collection of species, but as an ecosystem that evolves alongside us. Just like forests respond to climate change, our microbiome communities adapt to diet, stress, medication, and environment. Understanding this ecological framework may be key to preventing chronic disease.
For example:
- When dietary fiber is scarce, microbes shift to digesting mucus lining the gut weakening its protective barrier.
- Overuse of antibiotics resembles deforestation, wiping out beneficial microbes and allowing harmful ones to dominate.
- Introducing probiotics or dietary diversity works like reforestation, encouraging microbial recovery.
Future Directions in Microbiome Research
Microbiome science is still young but expanding rapidly. Emerging frontiers include:
- Next-gen sequencing: Improved tools to map rare or low-abundance microbes.
- Microbiome-gene interactions: Understanding how microbes turn human genes on or off.
- Artificial intelligence (AI): Predicting disease risk using big microbiome datasets.
- Microbiome therapeutics: Designer probiotics or microbiome engineering for targeted treatments.
Conclusion
The human microbiome is more than a biological curiosity it is a partner in health. By viewing it as a dynamic ecosystem, we gain a deeper understanding of how microbes influence disease, immunity, and even aging. The future of medicine may lie in cultivating this ecosystem wisely, through personalized nutrition, microbiome-based therapies, and lifestyle choices that nurture microbial diversity.
Frequently Asked Questions (FAQs)
What is the human microbiome?
The human microbiome is the community of trillions of microorganisms, including bacteria, viruses, fungi, and archaea, living in and on the human body. These microbes are essential for digestion, immunity, and overall health.
How do microbiomes affect immunity?
Microbiomes train and regulate the immune system. Beneficial gut bacteria promote immune tolerance, prevent overreactions, and reduce inflammation, protecting the body from infections and autoimmune diseases.
Can diet influence the microbiome?
Yes, diet greatly influences microbiome composition. High-fiber diets encourage beneficial microbes, while high-fat, low-fiber diets can promote dysbiosis. Fermented foods and plant-based diets support microbial diversity.
What are the benefits of a diverse microbiome?
A diverse microbiome improves digestion, strengthens immunity, regulates metabolism, supports mental health, and protects against harmful pathogens. Reduced diversity is linked to obesity, allergies, and chronic diseases.
How can I maintain a healthy microbiome?
To maintain a healthy microbiome, eat a varied diet rich in fiber and fermented foods, reduce unnecessary antibiotics, spend time in natural environments, manage stress, and maintain regular sleep patterns.
Does the skin microbiome affect overall health?
Yes, the skin microbiome acts as a protective barrier against pathogens, helps regulate immune responses, and interacts with environmental microbes to maintain skin health.
What is microbiome dysbiosis?
Dysbiosis is an imbalance in the microbial communities of the body, often due to poor diet, antibiotics, stress, or environmental factors. It can lead to digestive issues, inflammation, and susceptibility to infections.
Can microbiomes influence mental health?
Yes, gut microbes communicate with the brain via the gut-brain axis, influencing mood, stress response, and neurological conditions such as anxiety and depression.
Do environmental microbes affect the human microbiome?
Environmental microbes can colonize the human body, enhancing microbial diversity and supporting immune health. Exposure to natural environments, soil, and pets positively influences the human microbiome.
Are probiotics effective for improving microbiome health?
Probiotics can help restore and maintain beneficial microbes, especially after antibiotic treatment or during digestive disorders. However, effectiveness depends on the strain, dosage, and individual microbiome.